Blog
The Evolution of TMS: Advancements in Treating Depression and Beyond
- posted: Dec. 15, 2023
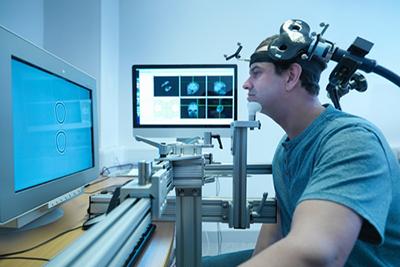
The Evolution of TMS: Advancements in Treating Depression and Beyond The physical principles of Transcranial Magnetic Stimulation or TMS have been in use for over 100 years, but the discovery of Read More
What Is NeuroStar TMS?
- posted: Dec. 13, 2023
What Is NeuroStar TMS Advanced Therapy? If you suffer from chronic depression, you already know how it can impact your life, causing you to not live the full, happy life you Read More
The Right OCD Treatment Option For You
- posted: Aug. 25, 2023
Obsessive Compulsive Disorder Treatment Obsessive-compulsive disorder, also known as OCD, is a complex disorder. A person with OCD will experience thoughts and fears which cause the person to perform repetitive actions, Read More
TMS Obsessive Compulsive Disorder Treatment
- posted: Jun. 13, 2023
Obsessive-compulsive disorder, also known as OCD, is a condition in which a person has recurrent, obsessive, distressing, unwanted thoughts. To relieve the thoughts, the person is driven to practice compulsive, Read More
What Is NeuroStar?
- posted: Jun. 13, 2023
If you suffer from depression, you’ve probably tried medication, counseling, lifestyle modification, and other treatment solutions. You may have had some relief from depression symptoms, only to find the relief Read More
How Antidepressants Work Vs. TMS
- posted: Jan. 25, 2023
Do you or a loved one struggle with depression? There are several types of treatment that doctors and psychiatrists recommend for depression. They often go in different stages. First, they may recommend Read More
NeuroStar TMS For Veterans
- posted: Jan. 25, 2023
VETERANS AND DEPRESSION According to the Department of Veterans Affairs, in 2008 one in three veterans visiting a primary care physician reported having symptoms of depression, while one in five reported experiencing Read More
TMS vs. ECT: What is the Difference?
- posted: Jul. 13, 2021
What is Transcranial Magnetic Stimulation (TMS) and what Electroconvulsive Therapy (ECT)? What is the difference between the two? Transcranial Magnetic Stimulation sounds terrifying. Electroconvulsive therapy sounds even more frightening. Both TMS and Read More
Will TMS Affect My Personality?
- posted: Jul. 09, 2021
There are several reasons that someone might require TMS treatment, whether you’ve got Autism or you’re one of the 300 million people that suffer from depression. One of the most Read More
The Link Between Stress and Depression
- posted: Jun. 30, 2021
Stress is not only commonplace in our daily lives; it’s normal. However, the degree of stress that we experience and its sustained nature can trigger depression in some individuals. Chronic stress, Read More
Living with Treatment-Resistant Depression
- posted: Jun. 24, 2021
Feeling sad or down every now and then is normal, and a part of everyday life. We all experience some moments of sadness, hopelessness, and even depression. If you get Read More
15 Coping Skills for Depression
- posted: Jun. 18, 2021
Being prescribed antidepressants that may or may not work for your depression is almost a slap in the face. When your doctor does not offer any practical advice for helping Read More
How Long Do The Effects Of TMS Treatment Last?
- posted: Jun. 16, 2021
Nearly seven percent of American adults struggle with depression each year. It’s a disease that can feel inescapable at times. When medications and therapy just aren’t getting the results you want, Read More
How Does Depression Affect The Brain?
- posted: Jun. 16, 2021
Around the world, there are more than 264 million people that suffer from depression. Depression can make it difficult for individuals to carry on with daily activities and is a Read More
Contact Us
Our Locations
Cedar Knolls Location
14 Ridgedale Ave Suite 103
Cedar Knolls, NJ 07927, US
Hours of Operation
9:00 am - 5:00 pm
9:00 am - 5:00 pm
9:00 am - 5:00 pm
9:00 am - 5:00 pm
9:00 am - 5:00 pm
Closed
Closed